Hypoxic load : a new index integrated into CIDELEC tools
Obstructive sleep apnoea-hypopnoea syndrome is responsible for cardiovascular complications involving dysfunction of the autonomic nervous system. However, because the standard measure used to assess the severity of OSAHS – the apnoea-hypopnoea index (AHI) – is not sufficient to predict cardiovascular risk and the risk of mortality, several teams have been working to define a new index that characterises hypoxia caused by respiratory events. This index is called the hypoxic load, which CIDELEC has chosen to integrate into its software to help sleep professionals optimise their diagnoses. Explanations.

Hypoxic load, a relevant index for assessing the risk of morbidity and mortality associated with OSAHS
The relevance of the diagnosis, and the practitioner’s ability to anticipate possible future complications, are two major challenges for patients suffering from sleep apnoea. In order to provide additional information and improve diagnoses of OSAHS, an American team has developed a method of calculating the image of the lack of oxygenation in the blood during the night: the hypoxic load.
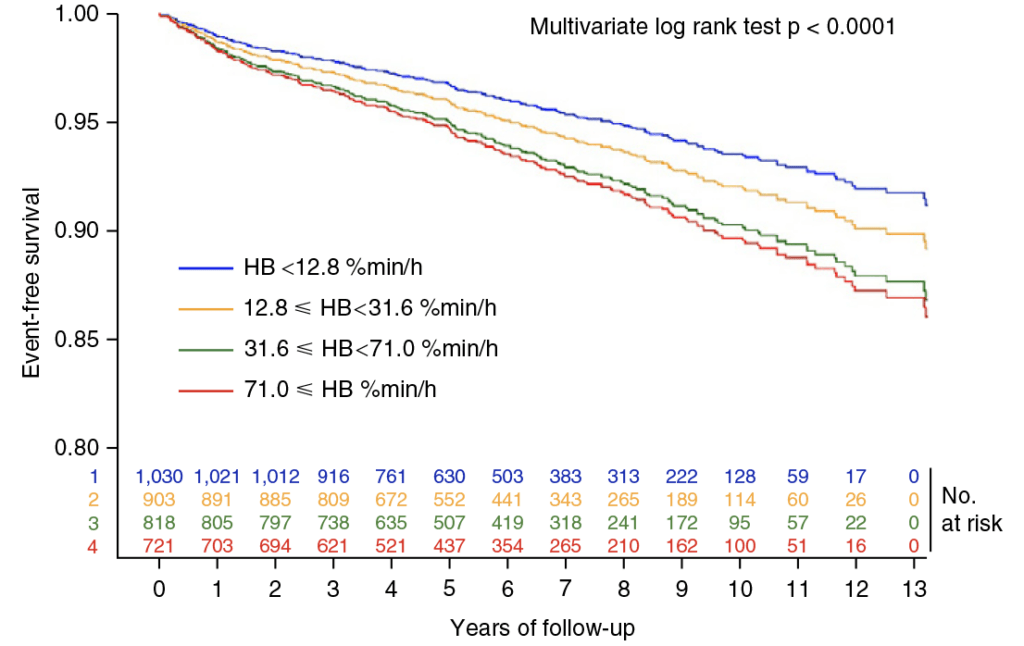
The American study, published in 2019 in the European Heart Journal, shows that hypoxic load predicts cardiovascular disease mortality in people suffering from OSAHS. It highlights the importance of taking into account the duration and intensity of desaturation caused by respiratory events, in addition to their frequency, when estimating the risk of developing cardiovascular disease. In addition, this study showed that a hypoxic load of over 71% min/h multiplied the cardiovascular risk by 1.62 in patients from the Sleep Heart Health Study (SHHS) cohort.
The study by Azarbarzin, Sands, Stone et al. quickly gained momentum and led to other publications, as well as more and more mentions at specialist conferences. CIDELEC quickly became interested in this new index as a tool to complement the diagnosis of sleep apnoea. Consequently, it was decided to launch new clinical investigations.
MACE: combined variable for stroke, myocardial infarction, heart failure and all-cause mortality. We felt that the work carried out on the cohort was sufficiently significant for us to decide to integrate the hypoxic load index into the CIDELEC software, with effect from 7 July 2022, especially as our tools were used to measure the hypoxic load in this research.
Investigating the hypoxic load
A team of doctors and researchers, including Professor Frédéric Gagnadoux, Head of Pneumology at Angers University Hospital and former President of the French Society for Sleep Research and Medicine (SFRMS), has carried out several studies on the subject.
For this purpose, a cohort of French patients monitored in several care centres in the Pays de la Loire region was used to measure the association of hypoxic load with the incidence of stroke in patients investigated for suspected sleep apnoea syndrome. It was set up by the region’s Respiratory Health Research Institute (IRSRPL),
of which some of the Angers CHU doctors who took part in the study are members.
In the first study, data from nearly 3,600 patients with no history of stroke were matched with data from the French National Health Data System (SNDS) to identify the possible occurrence of strokes. The study, published in the European Respiratory Journal in November 2020, clearly shows a correlation between lack of oxygen during the night and increased risk: patients with a high hypoxic load are at greater risk of developing a stroke.
This study showed that a hypoxic load of more than 45% min/h multiplied the risk of stroke by 2.59 compared with patients with a low hypoxic load. In addition, a subsequent study showed that a hypoxic load greater than 31.6% min/h significantly increased the risk of major cardiovascular events (MACE).
Hypoxic load in CIDELEC software
The hypoxic load is assessed automatically in the CIDELEC software. It is obtained by considering the areas under the desaturation curve associated with respiratory events.
Its value is shown in the recording summary, and a scale in the ‘Results graph’ tab makes it easier to interpret.
This scale is based on thresholds proposed in the literature.
An index to complement the apnoea-hyponoea index
The hypoxic load index complements the apnoea-hypopnoea index, which is unable to estimate the risk of morbidity and mortality in patients suffering from OSAHS. In the example below, two patients with the same AHI have very different hypoxic load values.

The hypoxic load index complements the apnoea-hypopnoea index, which is unable to estimate the risk of morbidity and mortality in patients suffering from OSAHS. In the example below, two patients with the same AHI have very different hypoxic load values.
As the study confirmed, hypoxic load gives a relevant indication of the risk associated with cardiovascular disease, particularly stroke. This should improve diagnosis and patient care.
In conclusion, the hypoxic load, calculated by taking into account desaturations due to respiratory events, has been shown to be relevant for estimating cardiovascular risk. However, to date there are no standardised calculation rules or recognised severity thresholds. This is why the value obtained must be considered in the light of the results in the literature.
This index, used in conjunction with the apnoea-hypopnoea index, is one of the biomarkers that enable a reliable, personalised diagnosis to be made. Meanwhile, research is continuing: measuring hypoxic load could, in the future, help doctors assess the risks associated with other pathologies.


